Introduction: What Is a Low FODMAP Diet?

The low FODMAP diet has gained significant attention as a promising approach to managing symptoms associated with irritable bowel syndrome (IBS). But what exactly is this eating plan, and how does it work? At its core, the low FODMAP diet eliminates certain types of carbohydrates that can cause digestive discomfort for many individuals. These carbs are poorly absorbed by the small intestine, leading them to ferment in the large intestine, which often results in bloating, gas, cramping, and changes in bowel movements.
Imagine walking into a grocery store with a list of foods you suddenly cannot consume anymore – items like wheat-based breads, creamy dairy products, and sweet fruits such as apples. This is what many people experience when they start the low FODMAP diet, but it’s not just about exclusion; it’s also about understanding your unique body’s responses to different types of food. The diet moves through three phases: restrictive elimination to identify problem foods, reintroduction to pinpoint personal tolerances, and maintenance to tailor a sustainable plan that balances symptom management with nutrition.
For those curious about the potential benefits beyond IBS, there is growing interest in whether the low FODMAP diet might offer relief for individuals dealing with inflammatory bowel disease (IBD). The intricate relationship between diet and digestive health raises intriguing questions: Could this dietary approach provide additional support alongside medical treatments? Might it help reduce flare-ups or improve overall quality of life for IBD sufferers?
Understanding how the low FODMAP diet functions sets the stage for exploring its broader implications, particularly in the context of inflammatory bowel disease. This introductory exploration aims to pique your curiosity and set the foundation for diving deeper into this fascinating topic.
How Does the Low FODMAP Diet Work?
The low FODMAP diet works by systematically reducing the intake of fermentable carbohydrates known as FODMAPs, which stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These types of carbs are found in a variety of common foods, including wheat products, certain fruits, vegetables, and dairy items. By minimizing these specific carbohydrates, the diet aims to alleviate symptoms commonly associated with IBS.
When FODMAPs enter the digestive tract, they can draw water into the intestines due to their osmotic properties, leading to bloating and discomfort. Additionally, because many people have difficulty digesting and absorbing FODMAPs efficiently, these sugars pass through to the large intestine where bacteria ferment them. This fermentation process produces gases such as hydrogen and methane, contributing further to symptoms like abdominal pain, flatulence, and diarrhea or constipation.
Understanding how different foods impact your body is crucial on a low FODMAP diet. For instance, lactose in milk products can be problematic for many people due to insufficient production of the enzyme lactase needed to break it down properly. Similarly, fructose, which is found naturally in fruits like apples and mangoes, or added to various processed foods, may cause issues if consumed in excess relative to glucose.
The elimination phase of the diet involves removing all high FODMAP foods for a period, typically two to six weeks. This strict phase helps identify which specific FODMAPs are causing symptoms by eliminating possible triggers completely. Following this restrictive period, individuals can begin a reintroduction phase where they systematically introduce different types of FODMAP-rich foods back into their diet while closely monitoring any resulting digestive reactions.
By carefully tracking symptom patterns during the reintroduction process, individuals can create personalized dietary plans that balance nutritional needs with symptom management. This tailored approach allows for more sustainable long-term adherence to the low FODMAP diet without unnecessary food restrictions.
The acronym “FODMAP” was coined by a team of researchers at Monash University in Australia who developed this dietary protocol as part of their research into IBS and other functional gastrointestinal disorders.
Recommended Foods for a Low FODMAP Diet
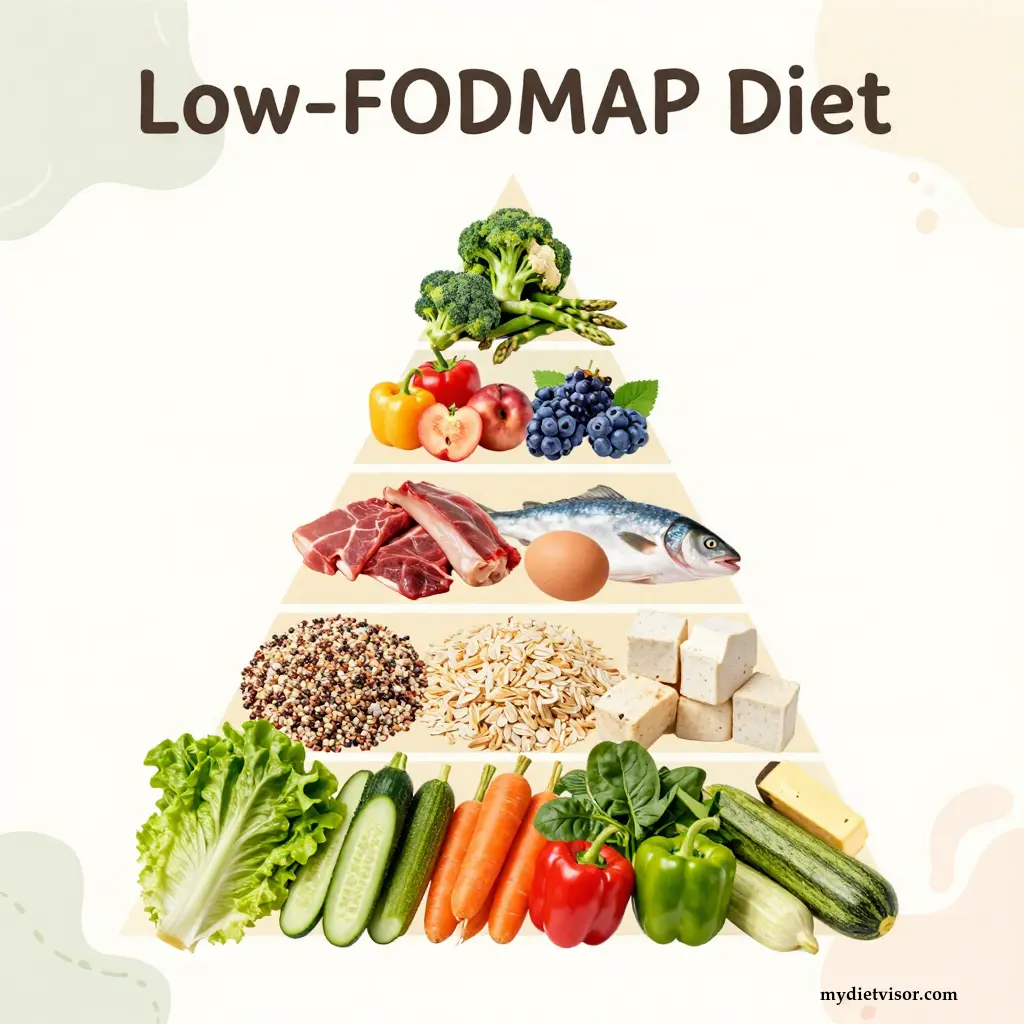
When embarking on a low FODMAP diet, it’s important to know which foods can be safely consumed during the elimination phase and beyond. This list includes a variety of fruits, vegetables, grains, proteins, and dairy alternatives that are generally well-tolerated by most people following this dietary approach.
Vegetables
Vegetables form an essential part of any healthy diet and are no exception on the low FODMAP plan. Choose from green beans, carrots, bell peppers (without seeds), cucumbers, lettuce, spinach, tomatoes, zucchini, and squash to enjoy a range of flavors and textures without triggering digestive symptoms. It’s important to note that some vegetables like broccoli, cauliflower, and onions are high in FODMAPs and should be avoided during the restrictive phase.
Fruits
Fruit lovers on a low FODMAP diet will find plenty of options to enjoy while adhering to dietary restrictions. Opt for bananas, blueberries, grapes, honeydew melon, oranges, strawberries (limited quantity), kiwi, and pineapple. These fruits offer the vitamins and antioxidants necessary for good health without overwhelming your digestive system with high FODMAP content.
Grains
Whole grains are a staple in many diets due to their nutritional benefits, but some can be challenging for individuals sensitive to FODMAPs. Brown rice, quinoa, millet, and oats (without added sugars or high-FODMAP ingredients) are excellent choices when following the low FODMAP diet. They provide fiber, protein, and other essential nutrients without causing digestive distress.
Proteins
Incorporating a variety of proteins into your meals is crucial for maintaining muscle mass and overall health. On a low FODMAP diet, lean meats like chicken, turkey, beef (trimmed of fat), fish, eggs, and tofu are great options. These foods not only supply protein but also add diversity to your meal plans, making it easier to stick with the dietary guidelines.
Dairy Alternatives
For those sensitive to lactose or other dairy components that contain FODMAPs, there are several non-dairy alternatives available. Almond milk, rice milk, and coconut yogurt can serve as suitable replacements for cow’s milk products. These options offer a creamy texture and some nutritional value without causing digestive issues.
Snacks and Condiments
Finding snacks and condiments that fit into the low FODMAP diet doesn’t have to be complicated or boring. Opt for nuts like macadamia, peanuts (without added sugars), seeds such as pumpkin seeds, and hummus made from low-FODMAP ingredients can keep your snack options interesting while staying within dietary limits.
Table Comparing High vs Low FODMAP Foods
| Category | Low FODMAP Example | High FODMAP Example |
|---|---|---|
| Vegetables | Green beans, carrots | Broccoli, cauliflower |
| Fruits | Bananas, blueberries, strawberries (limited) | Apples, mangoes |
| Grains | Brown rice, quinoa | Wheat-based breads |
| Proteins | Chicken, turkey, fish, eggs | Lentils |
| Dairy Alternatives | Almond milk, coconut yogurt | Cow’s milk, cheese |
| Snacks & Condiments | Peanuts (without added sugars), hummus | Cashews, black beans |
Understanding which foods to include in your diet can make the low FODMAP approach more manageable and enjoyable. By focusing on these alternatives, you can maintain a balanced intake of nutrients while effectively managing your digestive symptoms.
The Monash University Low FODMAP Diet app offers an extensive database of food items with their corresponding FODMAP content ratings, helping individuals navigate dietary choices more easily.
Understanding IBD: Crohn’s Disease vs. Ulcerative Colitis
Inflammatory bowel diseases (IBD) encompass a range of conditions characterized by chronic inflammation of the digestive tract. Two primary types, Crohn’s disease and ulcerative colitis, have distinct features and affect different parts of the gastrointestinal system.
Crohn’s Disease
Crohn’s disease can occur anywhere along the length of the digestive tract but is most commonly found in the ileum (the last part of the small intestine) or at the junction between the small and large intestines. Unlike ulcerative colitis, which primarily affects the colon, Crohn’s disease can cause inflammation that extends deep into the layers of the intestinal wall. This condition often leads to symptoms such as abdominal pain, diarrhea, fatigue, and weight loss.
Ulcerative Colitis
Ulcerative colitis, on the other hand, is confined to the large intestine (colon) and rectum. The inflammation typically affects only the innermost lining of these organs, causing ulcers that can bleed easily. Common symptoms include persistent diarrhea mixed with blood, abdominal pain, weight loss, and an urgent need for bowel movements.
Key Differences
| Feature | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Location | Any part of the digestive tract | Colon and rectum |
| Depth of Inflammation | Affects all layers of the intestinal wall | Limited to the innermost lining |
| Symptoms | Abdominal pain, diarrhea, fatigue, weight loss | Diarrhea with blood, abdominal pain, urgency |
Understanding these differences is crucial for both patients and healthcare providers. While symptoms can sometimes overlap, accurate diagnosis is essential in guiding treatment decisions and dietary recommendations like those involving a low FODMAP diet.
Both conditions are chronic and require ongoing management, often combining medication, surgery, and lifestyle changes to control symptoms and prevent complications. The role of dietary modifications, such as the low FODMAP approach, becomes increasingly important for managing functional gastrointestinal symptoms associated with IBD.
Personal Reflection
Have you ever felt overwhelmed by trying to manage your diet alongside medical treatments? Many individuals with IBD find that a structured dietary plan like the low FODMAP diet can make a significant difference in their daily lives. However, navigating this journey alone can be challenging and may require professional guidance from nutritionists or dietitians who specialize in these conditions.
By understanding the nuances between Crohn’s disease and ulcerative colitis, patients and healthcare providers are better equipped to tailor dietary interventions that not only manage symptoms but also improve overall quality of life.
Impact of Low FODMAP Diet on Inflammatory Bowel Disease Symptoms
The potential benefits of a low FODMAP diet for individuals suffering from inflammatory bowel disease (IBD) extend beyond just managing IBS symptoms. Research has shown that while the diet may not alter the underlying inflammation or disease progression, it can significantly improve digestive discomfort and quality of life for those with IBD.
Symptom Management
One of the primary reasons patients turn to a low FODMAP diet is its ability to alleviate common gastrointestinal symptoms such as bloating, gas, abdominal pain, and diarrhea. These symptoms are often more pronounced during flare-ups of Crohn’s disease or ulcerative colitis, making dietary adjustments crucial for symptom control.
Quality of Life Improvements
Living with IBD can be challenging due to the unpredictable nature of symptoms and their impact on daily activities. A study by Muir et al. (2015) found that individuals who followed a low FODMAP diet reported significant improvements in quality of life, including reduced stress levels and better overall well-being.
Patient Testimonials
Many patients have shared their personal experiences with the low FODMAP diet, highlighting both its benefits and challenges. For instance, Sarah, a 35-year-old patient with ulcerative colitis, found that adhering to this dietary plan helped her manage her symptoms more effectively during active disease states.
Challenges in Adherence
While the potential benefits are clear, maintaining adherence to a low FODMAP diet can be difficult for several reasons. The strict nature of the diet, which requires careful food selection and preparation, can lead to feelings of restriction and social isolation. Additionally, there is often confusion about interpreting nutritional labels and understanding which foods contain high levels of FODMAPs.
Role of Professional Guidance
Professional guidance from a registered dietitian or nutritionist who specializes in IBD can make all the difference in successfully implementing the low FODMAP diet. These experts provide personalized meal plans, educate on food labeling, and offer emotional support to help patients navigate dietary restrictions more effectively.
By working closely with healthcare providers, individuals can tailor their diets to better suit their unique needs while still reaping the benefits of reduced symptom severity and improved quality of life.
Future Directions
As interest in the low FODMAP diet continues to grow among IBD patients, further research is needed to understand its long-term effects on disease management. Investigating how dietary interventions interact with medical treatments could lead to more comprehensive care strategies that address both physical symptoms and emotional well-being.
In conclusion, while the low FODMAP diet does not cure or prevent inflammatory bowel diseases, it offers a valuable tool for symptom control and enhanced quality of life. With proper guidance and support, this dietary approach can be an integral part of a holistic treatment plan for individuals managing IBD.
The Monash University Low FODMAP Diet app has been downloaded over 1 million times globally, highlighting its popularity among those seeking relief from digestive discomfort.
Improving Quality of Life with Low FODMAP for IBS Symptoms
The low FODMAP diet is not only effective for managing symptoms associated with irritable bowel syndrome (IBS) but also holds promise for improving quality of life. By systematically eliminating foods high in fermentable carbohydrates, individuals can experience significant relief from bloating, gas, abdominal pain, and changes in bowel habits.
Living with IBS often means navigating a complex array of dietary restrictions to avoid triggering symptoms. The low FODMAP diet simplifies this process by categorizing common trigger foods and providing clear guidelines for what is safe to eat during different phases of the diet. This clarity can greatly reduce anxiety around meal planning, making it easier to enjoy social gatherings and maintain a balanced lifestyle.
Daily Life Adjustments
Adapting to a low FODMAP diet involves more than just swapping out high-FODMAP foods; it requires a holistic approach to eating habits and lifestyle choices. For instance, dining out at restaurants becomes an exercise in careful selection and communication with servers about dietary needs. Cooking from scratch allows greater control over ingredients but can be time-consuming.
Emotional Well-being
Beyond physical symptoms, the emotional toll of managing IBS cannot be underestimated. The unpredictable nature of digestive issues often leads to stress, anxiety, and a sense of helplessness. By adhering to a low FODMAP diet, individuals report feeling more in control of their health and experiencing improved mental well-being.
Social Aspects
Navigating social situations can become challenging when dietary restrictions are involved. However, with the structured nature of the low FODMAP diet, many find it easier to participate in communal meals without fear of triggering symptoms. This is particularly important for maintaining relationships and overall quality of life.
A study by Biesiekierski et al. (2013) found that up to 75% of IBS patients experienced significant improvements in their symptoms after following a low FODMAP diet, underscoring its effectiveness as an intervention for managing functional gastrointestinal disorders.
Incorporating the low FODMAP diet into daily life can transform the way individuals with IBS experience food and social interactions. By making informed choices and seeking professional guidance when needed, people can take proactive steps towards better health and a more enjoyable quality of life.
Challenges and Barriers to Implementing a Low FODMAP Diet
Switching to a low FODMAP diet is not without its challenges, especially for individuals already managing inflammatory bowel disease (IBD). One of the primary hurdles is the complexity of dietary restrictions. The diet requires cutting out numerous common foods that are high in fermentable carbohydrates, which can be overwhelming and confusing at first glance. Imagine trying to navigate a grocery store where many familiar items are suddenly off-limits – this adjustment period often leads to feelings of frustration and isolation.
Moreover, interpreting food labels is another significant barrier. Many processed foods contain hidden sources of FODMAPs that aren’t immediately obvious from the ingredient list alone. This necessitates a thorough understanding of nutritional information, which can be daunting for those new to dietary restrictions. For instance, many people are surprised to learn that certain fruits and vegetables they thought were healthy actually contain high levels of fructose or other fermentable sugars.
Social Challenges
Social situations also pose unique challenges when following the low FODMAP diet. Dining out at restaurants can become a stressful experience as individuals have to navigate menus carefully while avoiding common trigger foods. This often leads to feeling left out during social gatherings, especially those centered around food, such as potlucks or dinner parties.
Emotional Impact
The emotional toll of dietary restrictions should not be underestimated. The constant vigilance required to maintain the diet can lead to feelings of stress and anxiety. For IBD patients who already face significant mental health challenges due to their condition, these additional pressures can exacerbate existing issues like depression and isolation.
Financial Considerations
Adhering to a low FODMAP diet can also be costly. Opting for specialty foods that are compliant with the dietary guidelines often comes at a premium price. For instance, almond milk or coconut yogurt may be more expensive than their conventional counterparts. Additionally, seeking professional guidance from registered dietitians who specialize in IBD can add to the financial burden.
Importance of Professional Guidance
Given these challenges, having access to professional guidance becomes crucial for success on the low FODMAP diet. A registered dietitian or nutritionist trained in managing IBD and dietary restrictions can provide personalized meal plans, educate about food labeling, and offer emotional support. These professionals help bridge the gap between understanding the theoretical aspects of the diet and applying them practically in daily life.
Patient Testimonials
Many patients find that working closely with healthcare providers eases their transition into the low FODMAP lifestyle. For example, Mark, a 42-year-old patient with Crohn’s disease, mentioned that regular consultations with his nutritionist were instrumental in managing his symptoms effectively. He emphasized how structured meal plans and recipe suggestions made adhering to the diet more manageable.
By addressing these challenges head-on and seeking professional assistance, individuals can better navigate the complexities of a low FODMAP diet while reaping its benefits for symptom management and overall quality of life.
The Monash University Low FODMAP Diet app includes over 10,000 food items with their FODMAP content ratings, making it easier for users to make informed choices about what they eat.
Role of Dietitians in Supporting Patients on a Low FODMAP Diet
Dietitians play a critical role in supporting patients who adopt a low FODMAP diet, especially those dealing with inflammatory bowel disease (IBD). These healthcare professionals provide essential guidance that helps individuals navigate the complexities and challenges associated with dietary restrictions. A registered dietitian can offer personalized meal plans tailored to individual needs, which is particularly important given the unique nature of each person’s symptoms and triggers.
Personalized Meal Plans
One of the most significant benefits a patient receives from working with a dietitian is access to personalized meal plans. These plans not only address nutritional requirements but also help manage specific digestive issues. For example, a dietitian can provide detailed guidance on how to incorporate low FODMAP foods into daily meals while ensuring adequate intake of essential nutrients like fiber and protein.
Education and Label Interpretation
Educating patients about food labels is another crucial aspect of dietary support. Understanding the FODMAP content in various products can be challenging, especially when it comes to processed or prepared foods. A dietitian teaches patients how to read ingredient lists, identify hidden sources of fermentable carbohydrates, and make informed choices that align with their dietary restrictions.
Emotional Support
The emotional impact of adhering to a restrictive diet like the low FODMAP plan should not be overlooked. Many individuals experience feelings of isolation and stress as they navigate new dietary guidelines and social situations. Dietitians provide emotional support by addressing these concerns, helping patients build confidence in their ability to manage their condition through diet.
Practical Advice and Recipe Suggestions
Dietitians also offer practical advice on meal preparation and cooking techniques that align with the low FODMAP diet. This includes tips for shopping for compliant foods at grocery stores and suggestions for simple yet tasty recipes that fit within dietary guidelines. By providing such resources, dietitians empower patients to take control of their health while enjoying a varied and satisfying diet.
Collaborative Care
Effective management of IBD often involves a multidisciplinary approach combining medical treatments with lifestyle changes like dietary modifications. Dietitians work closely with gastroenterologists, primary care providers, and other healthcare professionals to create comprehensive treatment plans that address both physical symptoms and emotional well-being.
By integrating professional support from dietitians into their care regimen, individuals can more effectively manage the challenges posed by inflammatory bowel disease while improving their quality of life. The tailored guidance offered by these experts helps patients navigate dietary restrictions confidently, fostering a sense of empowerment and control over their health journey.
A survey conducted by the Academy of Nutrition and Dietetics found that 85% of patients felt more confident in managing their IBD symptoms after consulting with a registered dietitian specializing in gastrointestinal conditions.
Potential Risks When Following a Low FODMAP Diet
While the low FODMAP diet offers significant benefits for managing digestive symptoms, it also comes with potential risks and drawbacks that are important to consider. One of the primary concerns is nutritional deficiencies. Many high-FODMAP foods are rich in essential nutrients such as fiber, vitamins, minerals, and antioxidants. By restricting these foods, individuals may inadvertently reduce their intake of crucial elements necessary for overall health.
Nutritional Deficiencies
For instance, limiting fruits like apples and pears can result in lower intakes of vitamin C and potassium, both vital for immune function and heart health. Similarly, avoiding certain vegetables such as onions and garlic means missing out on key phytochemicals that offer protective benefits against various diseases. Over time, this dietary restriction could lead to deficiencies in fiber, which is important for maintaining digestive health.
Impact on Gut Microbiome
Another potential risk associated with the low FODMAP diet involves alterations to gut microbiota. While the fermentation of FODMAPs by bacteria can cause symptoms like bloating and gas, these same processes also play a critical role in nourishing beneficial gut microbes. By reducing fermentable substrates through dietary restrictions, there is a possibility of disrupting the balance within the intestinal ecosystem.
Long-term Effects
The long-term impact of prolonged adherence to the low FODMAP diet remains uncertain. While short-term studies suggest benefits for symptom management, the effects on chronic health conditions and overall digestive function over extended periods are still being investigated. There is a need for more research to fully understand how such restrictive diets might affect gut health and microbiome diversity in the long run.
Psychological Impact
Beyond physical health considerations, there are also psychological aspects to bear in mind when adopting a low FODMAP diet. The inherent strictness of this eating plan can lead to feelings of deprivation and social isolation. Many individuals report experiencing stress and anxiety due to the constant vigilance required to adhere to dietary guidelines.
Practical Challenges
Practical challenges such as navigating restaurant menus or finding suitable meal options in social settings add an extra layer of complexity. Dining out often becomes a stressful experience, as many common dishes contain high-FODMAP ingredients that need careful avoidance. This can impact quality of life and enjoyment during social interactions centered around food.
Importance of Professional Guidance
Given these potential risks, it is crucial for individuals to seek professional guidance from registered dietitians or nutritionists who specialize in gastrointestinal conditions. These experts provide invaluable support by offering personalized meal plans, educating on nutritional labeling, and addressing emotional concerns related to dietary restrictions.
By understanding both the benefits and risks associated with the low FODMAP diet, patients can make informed decisions about whether this approach is right for them. Collaborating closely with healthcare professionals ensures that any necessary adjustments are made to maintain a balanced and sustainable lifestyle while effectively managing digestive symptoms.
It’s important to remember that everyone’s body reacts differently to food, so what works well for one person may not be the best fit for another.
In conclusion, while the low FODMAP diet can offer significant relief from gastrointestinal discomfort, it is essential to weigh its potential benefits against possible risks. By carefully considering nutritional impacts and seeking professional guidance, individuals can navigate this dietary approach more safely and effectively.
Always consult with a healthcare provider before making any drastic changes to your diet or treatment plan for inflammatory bowel disease.
Summary: Key Takeaways on Managing IBD Symptoms with Low FODMAP
In conclusion, while the low FODMAP diet offers substantial benefits for managing functional gastrointestinal symptoms in individuals with inflammatory bowel disease (IBD), it does not directly impact disease activity or inflammation markers. The key takeaway is that this dietary approach can significantly alleviate bloating, gas, abdominal pain, and diarrhea, thereby improving overall quality of life. However, the challenges associated with adhering to such a restrictive diet, including nutritional deficiencies and social isolation, should not be overlooked. Professional guidance from registered dietitians who specialize in IBD plays a crucial role in ensuring that patients can navigate these complexities successfully. Future research should focus on gathering more qualitative data specific to IBD populations to better understand the long-term effects and patient experiences with the low FODMAP diet. By doing so, healthcare providers can offer tailored support and resources that address both the physical and emotional needs of those managing IBD through dietary interventions.
Frequently Asked Questions (FAQ)
Is the low FODMAP diet effective for inflammatory bowel disease (IBD)?
The low FODMAP diet is not shown to impact IBD disease activity or inflammation markers. However, it can improve gastrointestinal symptoms compared to controls.
Can a low FODMAP diet help with abdominal pain in IBD?
Yes, the low FODMAP diet may reduce abdominal pain intensity and duration for individuals experiencing functional gastrointestinal symptoms related to IBD.
Does following a low FODMAP diet affect diet quality?
Adhering to the low FODMAP diet can potentially impact diet quality. It is important to work with a dietitian who can help tailor the diet to individual needs, ensuring adequate nutrition.
How does a low FODMAP diet influence gut microbiome in IBD patients?
There are potential impacts on the gut microbiome when following a low FODMAP diet. However, studies specifically examining these effects in IBD patients are limited.
Can the low FODMAP diet improve quality of life for people with IBD?
While the primary benefit is seen in reducing gastrointestinal symptoms, improvements in overall quality of life have been observed but may vary among individuals due to diverse experiences and needs.
What challenges do people face when starting a low FODMAP diet?
Common challenges include difficulty identifying trigger foods, potential nutritional deficiencies, and social impacts on dining out or family meals.
Is the low FODMAP diet safe for long-term use in managing IBD symptoms?
Long-term adherence to the diet requires careful monitoring by healthcare professionals to prevent nutritional imbalances. It should not be considered a standalone treatment for IBD but can complement medical management of symptoms.
How does the low FODMAP diet compare to other dietary approaches for IBS and IBD patients?
Unlike some exclusion diets, the low FODMAP diet allows consumption from each core food group, minimizing nutritional impact when properly followed. However, its effectiveness varies between IBS and IBD conditions.
What role do dietitians play in supporting those on a low FODMAP diet for IBD management?
Dietitians provide essential dietary assessment, counseling, and monitoring to optimize adherence, tailor the diet according to individual needs, and mitigate negative impacts.
Are there any side effects of following a strict low FODMAP diet without proper guidance?
Strict adherence without professional guidance can lead to unintended nutritional deficiencies or social limitations. Regular consultations with healthcare providers are crucial for effective management.



