What Is a Low-Protein Diet and Why Would You Need One?

A low-protein diet involves reducing your intake of protein well below what is typically recommended for optimal health. This dietary approach can be a game-changer for individuals dealing with specific medical conditions or seeking to improve their overall well-being. But why would you need such a diet? Let’s dive into the reasons behind this unique nutritional strategy.
Imagine someone diagnosed with kidney disease, where the body struggles to process excessive protein efficiently. For these individuals, reducing protein intake can be like giving the kidneys a much-needed break. Similarly, liver dysfunction and certain metabolic disorders often benefit from lower protein consumption as it helps manage symptoms and improves overall health outcomes. The origins of low-protein diets trace back over a century to early nutritional studies by scientists like Carl von Voit and Russell Henry Chittenden, who laid the groundwork for understanding our body’s needs regarding this essential nutrient.
One common misconception is that plant-based proteins are inherently inferior due to their varying amino acid compositions compared to animal sources. However, modern research has shown us that a well-planned low-protein diet can incorporate a variety of high-quality plant-based proteins while still supporting health benefits. This means you don’t have to rely solely on animal products to meet your protein needs effectively.
So why choose a low-protein diet? It could be the key to unlocking better metabolic health, enhanced insulin sensitivity, and even longer-term health benefits without having to drastically cut down on your total calorie intake. As we delve deeper into this topic, you’ll discover how tweaking your dietary composition can lead to surprising improvements in various aspects of wellness.
Understanding Protein Requirements
Understanding the importance of protein requirements is crucial when considering a low-protein diet. The recommended daily intake varies based on age, sex, weight, and activity level, but an average adult typically needs about 0.8 grams of protein per kilogram of body weight. This general guideline, however, does not apply uniformly to everyone.
For instance, athletes or individuals with greater muscle mass may need more protein to support their higher energy expenditure and tissue repair. On the other hand, older adults might require slightly more protein (around 1 to 1.2 grams per kilogram) due to age-related changes in muscle metabolism and decreased efficiency of protein synthesis. These differences highlight why a one-size-fits-all approach isn’t effective when it comes to dietary recommendations.
When transitioning to a low-protein diet, understanding these nuances becomes even more critical. For example, reducing protein intake while ensuring adequate nutrition can be challenging but is vital for managing conditions like kidney disease. In such cases, a registered dietitian or healthcare provider can help tailor the diet to meet specific needs and monitor health outcomes effectively.
Moreover, it’s essential to recognize that cutting down on protein does not mean sacrificing overall nutritional quality. A low-protein diet can still be rich in other vital nutrients such as vitamins, minerals, and fiber from fruits, vegetables, whole grains, and healthy fats. This balance ensures that you’re receiving the necessary components for optimal health despite reducing your protein consumption.
Did you know that some of the world’s longest-living communities consume diets lower in protein compared to many Western dietary patterns? These areas, often referred to as Blue Zones, provide intriguing insights into how a balanced diet with moderate protein intake can contribute to longevity and well-being.
How Does a Low-Protein Diet Compare to Calorie Restriction?
Calorie restriction (CR) has long been studied for its potential health benefits, including extended lifespan and improved metabolic health. CR typically involves reducing overall caloric intake while maintaining adequate nutrition to avoid malnutrition. However, a low-protein diet offers an alternative approach that mimics the effects of CR without necessarily limiting total calorie consumption.
| Feature | Low-Protein Diet | Calorie Restriction (CR) |
|---|---|---|
| Primary Focus | Reducing protein intake while maintaining other nutrients. | Reducing overall caloric intake to a level lower than what is required for weight maintenance. |
| Impact on Weight and Metabolism | Promotes leanness by altering body composition without significantly reducing total calories consumed. | Leads to weight loss due to reduced energy intake, which can improve insulin sensitivity and metabolic health. |
| Bone Health Effects | May have both positive and negative effects on bone density depending on the balance of calcium intake and acid load. | Generally improves bone health by reducing oxidative stress and inflammation associated with excess caloric intake. |
A low-protein diet is particularly intriguing because it can achieve similar metabolic benefits to CR without requiring drastic reductions in calorie consumption. This means individuals who might struggle with severe hunger or nutrient deficiencies during strict CR can still benefit from improved insulin sensitivity, lean body mass maintenance, and overall health enhancements.
For example, a study on mice found that diets low in protein but balanced in other nutrients led to better metabolic outcomes compared to high-protein diets. These findings suggest that tweaking the macronutrient composition rather than total caloric intake might offer comparable benefits to CR for certain populations.
Moreover, Blue Zones – regions with exceptionally long-living inhabitants – provide real-world evidence supporting the notion of low-protein diets. People in these areas often consume a diet lower in protein (less than 10% energy) and higher in plant-based foods, which aligns well with the principles of a balanced low-protein dietary approach.
In essence, while both CR and low-protein diets aim to enhance health and longevity, the latter offers a flexible alternative that focuses on reducing protein intake rather than overall caloric restriction. This flexibility can make it more accessible and sustainable for many individuals looking to improve their metabolic health without drastically changing their eating habits.
Recommended Food Groups on a Low-Protein Diet
When transitioning to a low-protein diet, it’s essential to focus on food groups that can provide the necessary nutrients without excessive amounts of protein. These foods not only help manage symptoms and conditions but also support overall health by providing vital vitamins, minerals, and fiber.
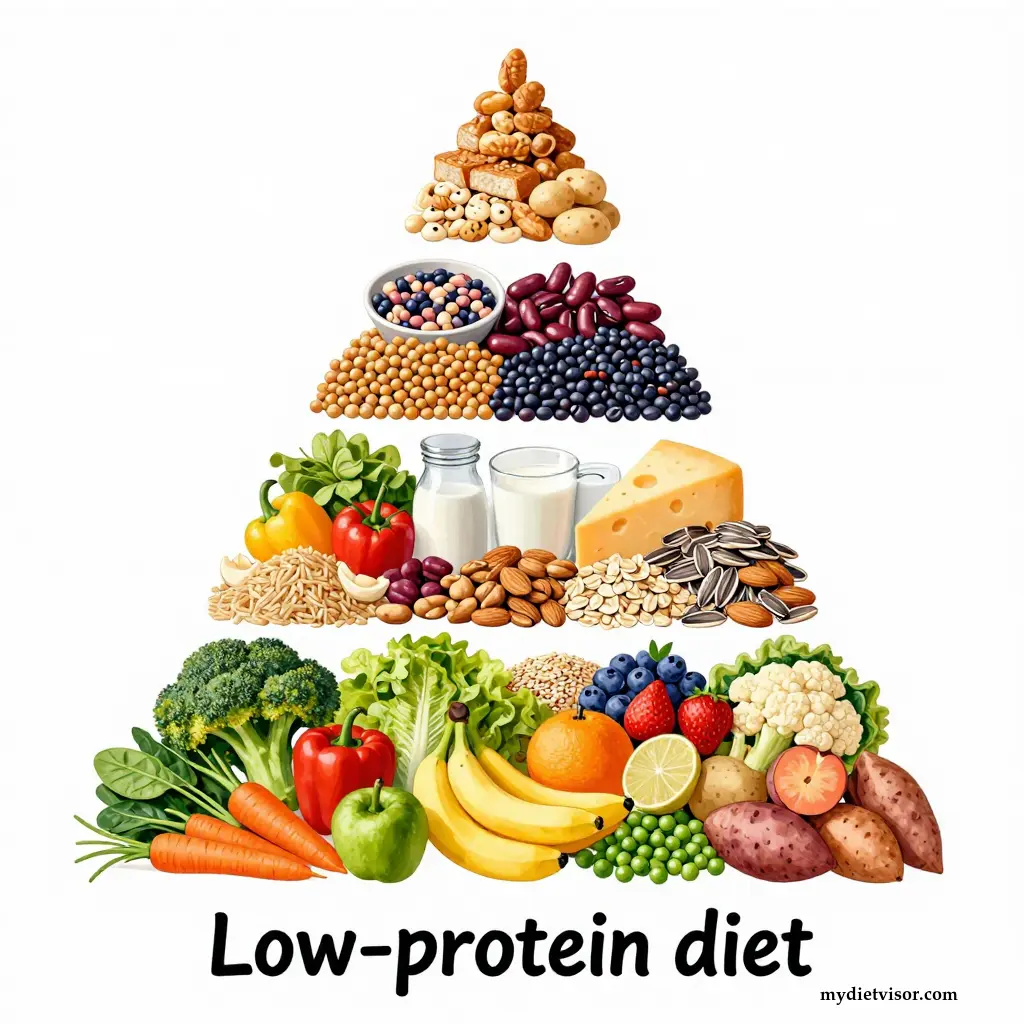
Vegetables and Fruits: Emphasizing vegetables and fruits is a cornerstone of any low-protein diet. Rich in essential vitamins, minerals, antioxidants, and dietary fiber, they play a crucial role in maintaining gut health and preventing chronic diseases. Aim for a variety of colors to ensure you’re getting a broad spectrum of nutrients. For instance, leafy greens like spinach and kale are excellent sources of iron and calcium without the high protein content found in meat.
Whole Grains: Whole grains such as brown rice, quinoa, oats, and barley offer complex carbohydrates that provide sustained energy throughout the day. They also contain a good amount of fiber, which helps regulate digestion and keeps you feeling full longer. Quinoa is particularly noteworthy for its complete amino acid profile, making it an ideal protein source on a low-protein diet.
Healthy Fats: Incorporating healthy fats into your meals can be beneficial in maintaining heart health and managing cholesterol levels. Foods like avocados, nuts, seeds, and olive oil are excellent choices as they provide essential fatty acids without contributing significantly to overall protein intake. These foods also help absorb fat-soluble vitamins such as A, D, E, and K.
Legumes: While legumes like beans and lentils contain some protein, they are predominantly carbohydrates and fiber. They can be a significant part of your diet for their nutritional value without overwhelming the protein content. For example, chickpeas provide iron, folate, and magnesium – important nutrients that contribute to energy production and immune function.
Dairy Alternatives: Traditional dairy products like milk, cheese, and yogurt are high in protein but can be replaced with plant-based alternatives such as soy milk, almond milk, or coconut milk. These substitutes not only reduce your protein intake but also provide essential vitamins and minerals needed for bone health, especially calcium and vitamin D.
Balancing these food groups ensures that you receive a comprehensive range of nutrients while adhering to the low-protein diet guidelines. It’s important to consult with a healthcare provider or registered dietitian to tailor this approach to your specific needs and medical conditions.
Wouldn’t it be fascinating if future studies reveal more precise dietary adjustments based on individual genetic makeup, further personalizing low-protein diets for optimal health benefits?
Forbidden or Limited Foods on a Low-Protein Diet
When embarking on a low-protein diet, certain foods must be avoided or consumed in very limited quantities to maintain the dietary guidelines. These restrictions are crucial for individuals managing specific health conditions such as kidney disease, liver dysfunction, or metabolic disorders.
Red Meat and Poultry: Red meat and poultry are prime examples of high-protein animal products that should be drastically reduced on a low-protein diet. These foods can contribute significantly to protein intake, which is counterproductive to the goals of a low-protein regimen. Instead, opt for leaner protein sources like fish or plant-based alternatives.
Dairy Products: Many dairy items are rich in protein and should be consumed sparingly or substituted with lower-protein options. Cheese, yogurt, milk, and cottage cheese all contain substantial amounts of protein. For instance, a cup of milk contains around 8 grams of protein. To adhere to your dietary plan, choose low-fat alternatives like almond milk or soy milk.
Eggs: Eggs are another high-protein food that needs moderation on this diet. A single large egg provides about 6 grams of protein, making it important to limit intake if your overall goal is to restrict protein consumption. Consider using egg whites or substitutes like tofu in recipes for a lower protein alternative.
Legumes (in Excess): While legumes such as beans, lentils, and chickpeas are nutritious due to their high fiber content and other essential nutrients, they also contain considerable amounts of protein. To avoid exceeding your daily protein limit, measure portions carefully or incorporate them in smaller quantities compared to typical serving sizes.
Protein Powders: Protein supplements like whey, casein, or soy protein powder should be avoided as these are designed specifically to increase protein intake. Replacing these with low-protein alternatives such as fruit smoothies blended with oats can provide a similar texture without the high protein content.
By focusing on forbidden and limited foods, you ensure that your diet remains within the recommended protein range while still providing necessary nutrients from other food groups. This careful selection not only aids in managing specific health conditions but also supports overall well-being by maintaining a balanced intake of essential vitamins and minerals.
Would it surprise you to learn that some cultures naturally consume diets low in protein, leading them to enjoy lower rates of chronic diseases compared to regions with higher protein consumption?
Does a Low-Protein Diet Affect Osteoporosis Risk?
Understanding how a low-protein diet affects osteoporosis risk requires delving into the intricate relationship between protein intake and bone health. Protein plays a dual role: it is crucial for building and maintaining strong bones, but excessive consumption can also lead to calcium loss.
On one hand, adequate protein intake supports skeletal integrity by providing amino acids necessary for collagen synthesis in bone tissue. Collagen forms the structural framework within bones that gives them strength and resilience. Without sufficient protein, this framework weakens, leading to a higher risk of fractures and osteoporosis. However, too much protein can have adverse effects.
High-protein diets, particularly those rich in animal proteins like meat and dairy, increase urinary calcium excretion as the body tries to neutralize the acidic load from metabolizing these proteins. This process may result in bone mineral loss if dietary calcium intake is insufficient to replace what’s being lost through urine. Over time, this can lead to weakened bones and an increased risk of osteoporosis.
In contrast, a low-protein diet might help mitigate some of these adverse effects by reducing the acid load on your body. This is because plant-based proteins tend to be less acidic compared to animal proteins. By incorporating more fruits, vegetables, and whole grains into your diet, you can maintain necessary protein levels while minimizing bone-damaging acids.
Furthermore, a balanced intake of calcium-rich foods alongside a moderate-protein diet can buffer the effects of acid production from dietary sources. For instance, leafy greens like kale and spinach are excellent plant-based sources of both calcium and vitamin K, which is vital for proper blood clotting and bone metabolism. Combining these with other low-protein foods helps ensure that your bones receive adequate nourishment without overloading on protein.
However, it’s important to note that drastically reducing protein intake can also be detrimental to bone health if not managed properly. Protein deficiency can impair collagen synthesis and disrupt the formation of new bone tissue, potentially leading to osteopenia or even osteoporosis over time. The key lies in finding a balanced approach where you meet your body’s needs for both calcium and protein while avoiding excessive intake that could negatively impact bone density.
In summary, the relationship between low-protein diets and osteoporosis risk is complex. While reducing protein consumption can help manage acid load and potentially reduce urinary calcium loss, it must be done cautiously to ensure adequate nutritional support for bone health. A well-balanced diet that includes a variety of plant-based proteins and sufficient calcium sources could offer a safer route towards maintaining strong bones while adhering to a low-protein regimen.
In populations where diets naturally contain less protein, such as the inhabitants of Okinawa in Japan, there is often lower incidence of age-related diseases including osteoporosis. This suggests that moderation in protein intake might be beneficial for long-term bone health.
Impact of Dietary Proteins on Metabolic Health
The effects of dietary proteins on metabolic health are multifaceted and can vary depending on the type and quantity of proteins consumed. High-protein diets, for example, have been widely studied for their potential to promote weight loss and enhance satiety due to their thermogenic effect and ability to increase feelings of fullness after meals.
On the other hand, a low-protein diet can offer distinct advantages in managing metabolic health by influencing insulin sensitivity and glucose regulation. Research indicates that reducing protein intake may improve glycemic control and reduce the risk of type 2 diabetes. This is particularly beneficial for individuals with prediabetes or early-stage diabetes who are looking to manage their condition without medication.
Another significant aspect of low-protein diets is their influence on lipid profiles. Studies have shown that lowering dietary protein can help decrease levels of triglycerides, LDL cholesterol, and improve the overall ratio of good (HDL) cholesterol to bad cholesterol. This positive impact on blood lipids contributes to reduced cardiovascular risk factors associated with metabolic syndrome.
Moreover, low-protein diets may also play a role in modulating inflammation within the body. Chronic inflammation is linked to numerous metabolic disorders including obesity, type 2 diabetes, and heart disease. By reducing protein intake, particularly from animal sources which are often higher in inflammatory compounds like arachidonic acid, individuals can potentially lower systemic inflammation markers such as C-reactive protein (CRP).
Understanding these dynamics helps highlight why tailoring dietary protein levels based on individual health profiles is crucial for optimizing metabolic outcomes. For someone looking to improve their metabolic health without resorting to strict calorie restriction, a low-protein diet might offer an effective and sustainable alternative.
How do you think adjusting your daily protein intake could impact your energy levels and overall well-being?
The Role of Essential Amino Acids in Weight Management
Understanding the role of essential amino acids (EAAs) within a low-protein diet is crucial for effective weight management and overall health. EAAs are vital because your body cannot produce them, so they must be obtained through food sources. These include histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine.
When considering a low-protein diet for weight management, it’s essential to ensure that you still receive all nine EAAs in adequate amounts. This balance helps maintain muscle mass while reducing body fat. For instance, leucine has been shown to activate mTOR pathways involved in protein synthesis, which is crucial for maintaining lean muscle tissue during calorie restriction or reduced protein intake.
Moreover, specific EAAs like lysine and methionine play a role in metabolic processes that support weight loss by enhancing thermogenesis and increasing satiety. Lysine, in particular, can help regulate appetite hormones such as ghrelin, which signals hunger to the brain. By modulating these hormones, you may feel fuller longer, reducing overall caloric intake without drastically cutting down on your food portions.
Incorporating a variety of plant-based protein sources that contain EAAs can be beneficial for those on a low-protein diet. Quinoa and soy products are excellent examples as they offer complete amino acid profiles. However, it’s important to note that relying solely on single-source foods might not provide all the necessary EAAs in balanced quantities.
Consulting with a healthcare provider or registered dietitian is crucial when planning your dietary regimen to ensure you’re meeting your nutritional needs while adhering to your low-protein goals. They can help create meal plans that include a mix of vegetables, whole grains, healthy fats, and plant-based proteins rich in EAAs.
Imagine how much easier it could be to manage your weight if your diet naturally included the right balance of essential amino acids without overloading on protein – wouldn’t that be ideal?
Neurological Regulation and Food Intake Control
Understanding how the brain regulates food intake is crucial for comprehending the effects of a low-protein diet on overall health. The hypothalamus plays a central role in this regulation by integrating various signals related to hunger, satiety, energy balance, and nutrient status.
The hypothalamic neuropeptides such as Neuropeptide Y (NPY) and Agouti-related protein (AgRP) stimulate food intake when the body senses energy deficiency or low blood glucose levels. Conversely, pro-opiomelanocortin (POMC) and Cocaine- and amphetamine-regulated transcript (Cart) act to suppress appetite and promote satiety.
These neuropeptides interact with each other through a complex network of feedback loops involving hormones like leptin, insulin, and ghrelin. For instance, when protein intake is low, the body may increase production of NPY and AgRP to stimulate hunger and encourage food consumption. This response helps the body compensate for reduced nutrient availability.
In the context of a low-protein diet, these mechanisms can be particularly relevant. By understanding how dietary changes affect neuropeptide signaling in the hypothalamus, researchers can better predict how such diets might influence appetite control, energy balance, and overall metabolic health.
Moreover, studies on mice have shown that varying levels of protein intake significantly impact the expression of these key regulatory genes within the hypothalamus. For example, a diet with 5% protein led to different hypothalamic gene expressions compared to diets containing 30% or 20% protein. This variability underscores the importance of dietary composition in modulating neural pathways involved in food intake and metabolism.
This intricate interplay between dietary protein levels and brain regulation highlights why a low-protein diet can be both beneficial and challenging depending on individual circumstances. It also suggests that tailoring such diets to specific physiological needs could offer personalized health benefits beyond general recommendations.
Do you think the way our body regulates food intake based on nutrient availability is an evolutionary adaptation or just a coincidence of biological development?
Mechanisms by Which Low-Protein Diets Influence Body Composition
Low-protein diets influence body composition through several physiological pathways that involve hormonal regulation, energy metabolism, and muscle protein synthesis. One of the key ways these diets work is by altering the levels of hormones like insulin-like growth factor 1 (IGF-1), which plays a critical role in promoting cell growth and differentiation, especially in muscles.
When you reduce your protein intake, IGF-1 levels tend to decrease, leading to reduced muscle protein synthesis. This can initially seem counterproductive for those aiming to maintain or build muscle mass. However, it also means less overall anabolic activity that could otherwise lead to excessive calorie storage as fat. By lowering IGF-1 and other growth factors like mTOR (mechanistic target of rapamycin), the body shifts its focus from building new tissue to maintaining existing structures more efficiently.
Additionally, low-protein diets can influence lipid metabolism by reducing circulating levels of branched-chain amino acids (BCAAs). High BCAA levels are often associated with insulin resistance and obesity. By lowering these levels through reduced protein intake, you may improve insulin sensitivity and glucose regulation, which in turn aids in managing body fat.
Another mechanism involves the reduction of urea production, a byproduct of protein breakdown that requires energy to excrete. Lowering urea formation means less energy is used for this process, potentially leading to more efficient use of calories for other metabolic processes such as fat oxidation and muscle maintenance.
It’s worth noting that while these mechanisms can be beneficial in managing weight and improving metabolic health, they must be balanced carefully. Severely restricting protein could lead to malnutrition if not done thoughtfully with guidance from a healthcare professional or registered dietitian.
How do you think the reduction of growth factors like IGF-1 might affect your long-term muscle mass when following a low-protein diet?
Summary: Key Takeaways from the Effects of Low-Protein Diets
In summary, low-protein diets offer a unique approach to managing various health conditions and improving overall well-being without the need for severe calorie restriction. From their historical roots established by pioneers like Carl von Voit and Russell Henry Chittenden to modern applications in treating kidney disease, liver dysfunction, and metabolic disorders, these diets have shown promising effects on body composition, insulin sensitivity, and longevity. While reducing protein intake can influence bone health and hormonal regulation, the key lies in balancing this reduction with adequate nutrient absorption and maintaining essential amino acid levels. The flexibility of low-protein diets allows for tailored nutritional plans that accommodate individual needs, making them a valuable tool in holistic health management. As research continues to explore the intricate mechanisms at play, understanding these dietary interventions can pave the way for personalized nutrition strategies that enhance quality of life.
Frequently Asked Questions (FAQ)
What are some potential risks associated with a low-protein diet?
A low-protein diet can pose certain risks if not properly managed. These may include an increased risk of osteoporosis due to calcium loss from bones, especially when protein intake is below the recommended level.
Can a low-protein diet help with weight management?
While some studies suggest that low-protein diets might aid in weight management by reducing appetite and improving satiety, it’s important to balance this approach carefully as too little protein can also lead to muscle loss and other health issues.
Are there any groups of people who should avoid a low-protein diet?
Certain populations, such as pregnant women, athletes undergoing intense training, or individuals with specific medical conditions, might require higher amounts of protein and thus could benefit less from a low-protein dietary regimen. Always consult a healthcare professional before starting a new diet.
How does a low-protein diet affect muscle growth and repair?
Muscle tissue requires adequate protein to grow and repair properly. A diet too low in protein may hinder recovery after exercise and impair the process of building lean muscle mass, which is important for overall health and wellness.
What are some common misconceptions about low-protein diets?
One common misconception is that all protein sources must be perfectly combined or paired with certain foods to maximize their benefits, a notion often associated with specific diet plans rather than scientific evidence. Another misconception is that high protein alone can solve obesity issues without considering other dietary and lifestyle factors.
How do I know if my body needs more or less protein?
Determining your personal protein requirement depends on various factors including age, gender, activity level, muscle mass goals, and overall health status. Consulting with a dietitian or healthcare provider is crucial to tailor recommendations that fit individual needs accurately.
Can low-protein diets affect blood sugar levels?
Research suggests that the impact of a low-protein diet on blood glucose management might vary; however, the primary determinant remains calorie balance rather than protein content alone. Proper carbohydrate and fat intake alongside sufficient physical activity should be considered for optimal glycemic control.
What are some easy ways to incorporate more plant-based proteins into my meals?
Including diverse sources of legumes like lentils and chickpeas, whole grains such as quinoa and brown rice, nuts, seeds, and soy products can easily enhance protein intake while maintaining a balanced diet rich in essential nutrients.
How does a low-protein diet influence hormonal balance?
The impact on hormones is an area of ongoing research. Some studies indicate that altering dietary components like protein might affect hormone levels involved in appetite regulation and metabolism, although the exact mechanisms are still being studied.
Are there any long-term health benefits to following a low-protein diet?
Long-term adherence to a low-protein diet may offer some metabolic advantages for certain individuals, but extensive research is needed to understand its full implications over extended periods. Balancing protein intake with other nutritional aspects remains key for overall health maintenance.



