The Impact of Sodium Intake on Congestive Heart Failure (CHF) Management

Low sodium diet has long been a cornerstone recommendation for individuals with congestive heart failure (CHF), aimed at reducing fluid buildup and alleviating symptoms such as swelling and shortness of breath. However, recent research is challenging this conventional wisdom by investigating whether moderate levels of sodium might actually benefit CHF patients more than strict restrictions.
The study in question involved 232 participants across various stages of heart failure severity, ranging from mild to severe cases (NYHA class II–IV). These individuals were monitored over a six-month period to determine the impact of different sodium intake levels on their hospital readmission rates. The two dietary approaches compared were normal-sodium consumption at 120 mmol versus low-sodium consumption at 80 mmol daily.
One of the key findings is that overly restrictive sodium diets may actually harm CHF patients more than help them. Patients often avoid not only high-salt foods but also other important nutrients and fluids, potentially leading to malnutrition or dehydration. These conditions can exacerbate heart failure symptoms by weakening cardiac muscle function and disrupting fluid balance within the body.
Another critical point highlighted in this research is how restrictive dietary guidelines might inadvertently increase hospital readmissions among CHF patients. By limiting sodium intake too strictly, healthcare providers may overlook the importance of maintaining a balanced diet that supports overall health and prevents further complications associated with heart failure. This shift in perspective underscores the need for personalized treatment plans rather than blanket recommendations.
This research raises questions about how we approach dietary management for CHF patients and encourages us to rethink traditional advice. It suggests that a moderate sodium intake might offer more holistic benefits, balancing the reduction of fluid retention with the maintenance of vital nutrients and fluids essential for heart health. This nuanced understanding challenges healthcare professionals to consider individual patient needs when formulating diet plans.
By prompting a reevaluation of current dietary guidelines for CHF management, this study opens up new avenues for improving patient outcomes through tailored nutritional strategies. It highlights the importance of considering each person’s unique medical history and lifestyle factors in developing effective heart failure care plans.
How Does Normal-Sodium Diet Compare to Low-Sodium Diet for CHF Patients?
When it comes to managing congestive heart failure (CHF), the conventional wisdom has long been that a low-sodium diet is best. However, recent research challenges this notion by examining how a normal-sodium diet compares to a low-sodium diet for patients with compensated CHF.
The study involved 232 participants aged between 55 and 83 years old, including both males and females. These individuals were classified under New York Heart Association class II–IV severity levels, indicating varying degrees of heart failure symptoms. The research aimed to assess the effects of sodium intake on readmission rates for CHF over an 180-day follow-up period.
Dietary Sodium Levels
Participants were divided into two groups based on their dietary sodium intake:
- Normal-Sodium Diet: Consuming approximately 120 mmol of sodium daily.
- Low-Sodium Diet: Adhering to around 80 mmol of sodium per day.
The study’s primary objective was to evaluate how these different levels of sodium consumption impacted hospital readmissions for CHF over the six-month period.
Key Findings
Contrary to traditional recommendations, the research did not find a significant difference in readmission rates between patients on normal-sodium and low-sodium diets. This challenges previous assumptions that reducing sodium intake is universally beneficial for managing heart failure.
The results suggest that strict sodium restrictions may not always be necessary or optimal for preventing hospitalizations among compensated CHF patients. Instead, the study highlights the need for personalized dietary recommendations based on individual patient characteristics such as age, gender, and severity of heart failure.
Implications
These findings prompt healthcare providers to reconsider their approach to sodium intake in heart failure management. By focusing on balanced dietary patterns tailored to each patient’s specific needs, rather than a one-size-fits-all low-sodium diet, better outcomes may be achieved for CHF patients.
While reducing sodium can help lower blood pressure in some individuals, overly restrictive diets might not be necessary or optimal for everyone’s health needs, especially when managing complex conditions like heart failure.
Recommended Foods on a Low-Sodium Diet
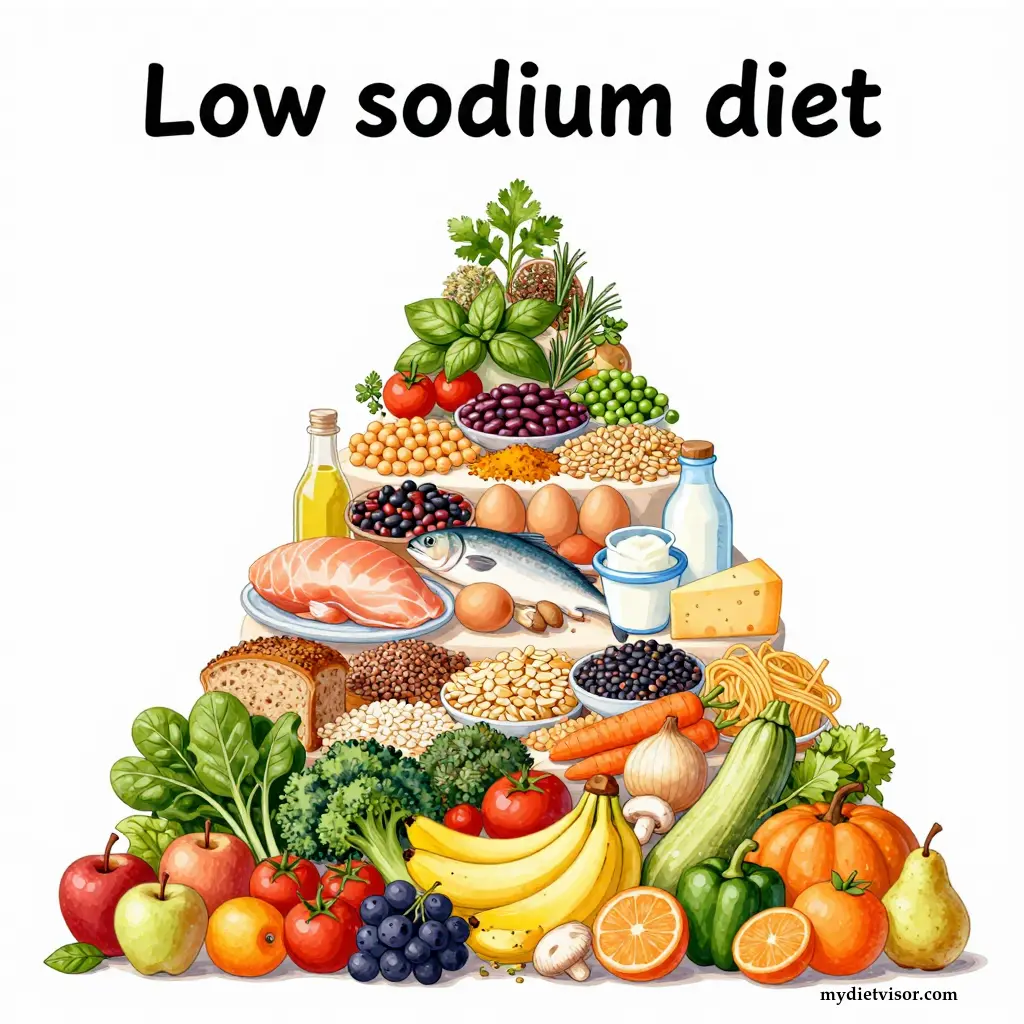
For a low-sodium diet, focusing on fresh, whole ingredients is key. Below is an extensive list of permitted foods grouped based on their role in maintaining a healthy sodium intake:
Foods to Consume in Abundance (Daily Basis)
These are the core components that form the foundation of your meals and snacks.
Fruits
Apples
Bananas
Berries (strawberries, blueberries, raspberries)
Grapes
Oranges
Pears
Vegetables
Leafy greens (spinach, kale, lettuce)
Cruciferous vegetables (broccoli, cauliflower, cabbage)
Bell peppers
Carrots
Zucchini
Squash
Sweet potatoes
Onions and garlic
Mushrooms
Tomatoes
Whole Grains
Brown rice
Quinoa
Oats
Barley
Buckwheat
Whole wheat bread (low sodium)
Whole grain pasta
Foods to Consume in Moderation (Limited Amounts Daily Basis)
These items provide essential nutrients but should be consumed with caution due to their sodium content.
Lean Proteins
Skinless chicken breast
Turkey
Fish (salmon, cod, tilapia) – choose fresh over canned or smoked varieties.
Eggs and egg whites
Dairy Products
Low-fat milk
Yogurt (unsweetened)
Cheese (low-sodium options)
Legumes
Lentils
Chickpeas
Black beans
Kidney beans
Peas
Foods to Use Sparingly or in Small Amounts as Seasonings and Additives
These ingredients add flavor while limiting sodium intake.
Herbs, Spices, and Low-Sodium Condiments
Fresh herbs (parsley, cilantro, basil)
Dried herbs (oregano, thyme, rosemary)
Ground spices (cumin, turmeric, black pepper)
Lemon juice or zest
Vinegar (balsamic, apple cider)
Fats and Oils
Olive oil
Avocado oil
Coconut oil
Beverages
Water
Unsweetened tea
Herbal teas
Sparkling water without added sodium
This list emphasizes the importance of choosing fresh ingredients over processed foods to manage your sodium intake effectively. Always check food labels and opt for products labeled as low-sodium or no salt added, especially when it comes to canned goods, condiments, and packaged meals.
Does Increasing Sodium Consumption Reduce Readmissions for CHF?
Recent studies are reevaluating the impact of dietary sodium levels on readmission rates for patients with compensated congestive heart failure (CHF). One such study compared the effects of normal-sodium and low-sodium diets over an 180-day period, involving 232 participants who were classified under New York Heart Association class II–IV.
- Study Design: The research involved a comparison between two dietary sodium levels: 120 mmol for the normal-sodium diet versus 80 mmol for the low-sodium diet. Participants included both males and females aged between 55 to 83 years old, representing different stages of CHF severity.
- Key Findings: The study’s results suggest that a moderate sodium intake might actually reduce hospital readmissions compared to severely restricting salt consumption. This challenges conventional advice recommending extremely low-sodium diets for heart failure patients.
By considering these findings, healthcare professionals are encouraged to adopt more personalized dietary recommendations based on individual patient needs rather than following generalized guidelines. These tailored approaches can lead to better health outcomes and improved quality of life for CHF patients.
The body requires sodium for various physiological functions, including nerve signal transmission and muscle contraction. However, excessive intake can strain the heart, especially in individuals with pre-existing conditions like CHF.
The impact of dietary sodium on hospital readmissions among patients with congestive heart failure (CHF) is a topic under close scrutiny by researchers. A recent study compared normal-sodium diets to low-sodium diets for 180 days, involving 232 participants from diverse age groups and stages of CHF severity.
Participants: The research included both male and female patients aged between 55 to 83 years old.
Dietary Intake Levels:
- Normal-sodium diet: Approximately 120 mmol daily
- Low-sodium diet: Around 80 mmol daily
The study’s key findings indicate that normal-sodium diets may be more effective than low-sodium diets in reducing readmission rates for CHF patients. This discovery challenges traditional dietary guidelines, which often recommend drastically limiting salt intake to manage heart failure symptoms.
These results highlight the need for a nuanced approach to managing sodium intake in CHF treatment plans. Personalized dietary recommendations can lead to better health outcomes and reduce healthcare burdens associated with frequent hospitalizations.
Sodium is vital for maintaining fluid balance and supporting nerve function, but excessive consumption can exacerbate heart conditions like CHF, illustrating the importance of balanced dietary advice.
The Role of Normal-Sodium Diets in Preventing CHF Readmissions
Recent research suggests that a normal-sodium diet might be more effective than a low-sodium diet in preventing hospital readmissions for congestive heart failure (CHF). This study examined two groups of participants – those on a normal-sodium diet and those adhering to a low-sodium diet – for 180 days.
Participants: The research involved 232 patients, aged between 55 to 83 years old, who were classified under New York Heart Association class II–IV based on their heart failure severity.
Dietary Intake Levels:
- Normal-sodium diet: About 120 mmol daily
- Low-sodium diet: Around 80 mmol daily
The study’s findings reveal no significant difference in readmission rates between the two dietary groups. This challenges the long-held belief that strictly limiting sodium intake is universally beneficial for CHF patients.
Understanding these results can help healthcare providers develop more effective and personalized treatment strategies, potentially reducing hospitalization rates and improving overall quality of life for heart failure patients.
Sodium plays a crucial role in nerve signaling and muscle function. While excess sodium can be harmful, moderate consumption may support better health outcomes for certain conditions like CHF.
Impact of Normal-Sodium Diets on Heart Failure Readmissions
Recent research challenges the notion that low-sodium diets are always best for managing congestive heart failure (CHF). A study compared normal-sodium and low-sodium diets over 180 days, involving 232 participants with varying degrees of CHF severity.
Participants: The study included both male and female patients aged between 55 to 83 years old.
Dietary Intake Levels:
- Normal-sodium diet: Approximately 120 mmol daily
- Low-sodium diet: Around 80 mmol daily
Key findings indicate that a normal-sodium diet did not lead to higher readmission rates compared to a low-sodium diet among CHF patients. This challenges the conventional wisdom of severely restricting sodium intake for heart failure management.
These insights highlight the importance of personalized dietary recommendations tailored to individual patient needs, rather than following blanket guidelines. Such an approach can optimize treatment outcomes and reduce healthcare utilization for those living with CHF.
While excessive sodium intake can be detrimental to heart health, moderate consumption might offer benefits that are overlooked in strict low-sodium diets for CHF patients.
Understanding the Effects of Different Sodium Levels on CHF Outcomes
A recent study explores how varying levels of dietary sodium influence readmission rates for congestive heart failure (CHF) among patients with compensated heart failure. The research compares the effects of a normal-sodium diet, containing 120 mmol of sodium daily, against a low-sodium diet at 80 mmol over an 180-day period.
Key findings from this study challenge conventional wisdom about sodium consumption in CHF management:
- Objective: The primary goal was to assess how dietary sodium levels impact readmission rates for patients with compensated heart failure.
- Study Design: Researchers followed 232 participants, including both males and females aged between 55 to 83 years old. Participants were categorized based on their New York Heart Association class II–IV severity levels.
The results indicate that a normal-sodium diet could be more effective than a low-sodium diet in reducing hospital readmissions for CHF patients with compensated heart failure. This suggests that strict sodium restrictions may not always benefit all individuals and highlights the need for personalized dietary recommendations based on individual patient characteristics.
Reconsidering Sodium Intake Guidelines
Traditionally, healthcare providers recommend severely restricting salt intake to manage symptoms of heart failure. However, this study proposes a more nuanced approach:
- Dietary Recommendations: A balanced diet with moderate sodium levels might be preferable to extremely restrictive diets for some patients.
- Quality of Life Considerations: Personalized dietary plans could improve the quality of life for CHF patients by allowing them more flexibility in their food choices.
By rethinking traditional guidelines, healthcare professionals can tailor treatment plans that are both effective and sustainable. This shift acknowledges the complexity of managing heart failure and emphasizes the importance of individualized care strategies.
Balancing Sodium Intake
Balancing sodium intake is crucial for maintaining overall health:
- Essential Role of Sodium: Sodium plays a vital role in nerve function, muscle contractions, and fluid balance.
- Moderation Key: While some sodium is necessary, excessive consumption can exacerbate heart conditions like CHF.
This balancing act underscores the need for tailored dietary advice that considers individual needs rather than applying broad generalizations. By understanding the nuanced impact of sodium on different patients, healthcare providers can develop more effective management strategies for CHF.
Sodium helps maintain proper fluid balance in our bodies; however, too much sodium can lead to water retention and increased blood pressure, which is particularly risky for individuals with heart conditions like CHF.
Normal vs. Low Sodium: Which is Better for Managing Heart Failure Symptoms?
Sodium intake plays a critical role in managing congestive heart failure (CHF), but the conventional wisdom of limiting salt may not always be the best approach. A recent study compared the effects of normal-sodium and low-sodium diets on readmission rates for patients with compensated CHF over 180 days. The research involved 232 participants, including both males and females aged between 55 to 83 years, who were classified as New York Heart Association class II–IV, indicating varying levels of heart function severity.
Key findings from the study suggest that a normal-sodium diet (120 mmol sodium) may be more beneficial than a low-sodium diet (80 mmol sodium) in reducing hospital readmissions for CHF. This challenges traditional dietary guidelines which often recommend restricting salt intake to manage heart failure symptoms. The research highlights the need for personalized nutritional strategies tailored to individual patient needs rather than a one-size-fits-all approach.
Doctors and nutritionists are rethinking their advice based on these results, considering factors like age, gender, and severity of CHF when recommending sodium levels in a diet plan. This shift in thinking aims at improving heart health outcomes while enhancing the quality of life for those living with CHF.
Keep in mind: The human body needs some sodium to function properly; it helps maintain fluid balance and supports nerve and muscle function. However, excessive intake can lead to complications like high blood pressure and heart issues, which is why balanced dietary advice is crucial.
How Does Normal-Sodium Diet Compare to Low-Sodium Diet for CHF Patients?
When it comes to managing congestive heart failure (CHF), the conventional wisdom has long been that a low-sodium diet is best. However, recent research challenges this notion by examining how a normal-sodium diet compares to a low-sodium diet for patients with compensated CHF.
In a study involving 232 participants aged 55 to 83 years old, researchers found no significant difference in readmission rates for heart failure between those on a normal-sodium diet and those on a low-sodium diet over an 180-day follow-up period. This suggests that the traditional approach of severely restricting sodium intake may not be as beneficial as previously thought.
Participants were divided into two groups: one following a normal-sodium diet with 120 mmol of sodium per day, while the other adhered to a low-sodium diet with only 80 mmol daily. The study focused on patients classified under New York Heart Association class II–IV, indicating varying levels of heart failure severity.
This research highlights that managing CHF is more nuanced than simply limiting salt intake. Instead, it suggests focusing on overall dietary patterns and lifestyle changes, which may include a balanced diet with moderate sodium consumption rather than stringent restrictions. This new perspective could lead to more effective and sustainable treatment plans for individuals dealing with chronic heart failure.
While reducing sodium can help lower blood pressure in some people, overly restrictive diets might not be necessary or optimal for everyone’s health needs, especially when managing complex conditions like CHF.
Summary: The Importance of Tailored Dietary Approaches for CHF Patients
Tailored dietary approaches are crucial for managing congestive heart failure (CHF), as highlighted by recent studies. The article examines the effects of different sodium intakes on readmission rates for patients with compensated CHF over an 180-day follow-up period, involving a total of 232 participants across various stages of CHF severity.
Objective: The study’s main goal is to evaluate how sodium intake impacts readmissions for CHF patients.
Study Details:
Duration: Six months of follow-up period.
Participants: 232 individuals diagnosed with compensated CHF, including both males and females aged between 55 and 83 years old.
Severity Classification: Patients were categorized based on their New York Heart Association (NYHA) class II–IV severity levels, indicating varying degrees of heart failure symptoms. This classification also included different ejection fractions among the participants.
The findings from this research challenge traditional views about sodium consumption in CHF management. Traditionally, low-sodium diets have been recommended to reduce fluid retention and lower blood pressure, which are known risks for exacerbating CHF. However, the study suggests that a moderate intake of sodium might be more effective than extremely restrictive diets in reducing hospital readmissions.
For example, patients on a normal-sodium diet (120 mmol) showed no significant increase in readmission rates compared to those adhering to a low-sodium diet (80 mmol). This indicates that the conventional wisdom recommending strict sodium restrictions may not be universally beneficial for all CHF patients. Instead, individualized dietary plans tailored to specific patient needs are likely more effective.
Moreover, this research underscores the importance of personalized dietary advice rather than one-size-fits-all recommendations. Tailored approaches can help optimize treatment outcomes and improve quality of life for patients with CHF by addressing their unique health profiles and conditions.
In summary, managing heart failure through sodium intake requires a nuanced understanding of individual patient needs. This study prompts healthcare providers to rethink their dietary guidelines for CHF management, moving towards more personalized nutritional strategies that balance the risks and benefits of different sodium levels.
Frequently Asked Questions (FAQ)
Is a low-salt diet really necessary for everyone with heart failure?
Not necessarily; the benefits of a low-sodium diet vary depending on individual health conditions and needs. Some people may benefit more from a normal-sodium diet tailored to their specific medical requirements.
How can I reduce my sodium intake without completely cutting out salt?
You can gradually lower your sodium by choosing fresh produce, reading labels carefully, cooking from scratch with low-sodium ingredients, and substituting high-sodium foods for healthier options.
Will increasing my daily salt intake help if I have heart failure?
For some people with heart failure, moderate sodium consumption (around 2,300 mg per day) may be better tolerated than extremely restrictive diets. However, this should only be done under medical supervision.
Can a high-sodium diet cause heart problems even if you don’t have heart failure?
Yes, consuming too much salt can raise blood pressure, which is a risk factor for developing heart disease and stroke, regardless of whether someone has pre-existing heart conditions.
What are some tips for sticking to a reduced sodium diet when eating out?
When dining at restaurants, choose meals that highlight fresh ingredients over processed foods. Opt for steamed or grilled options and ask your server about preparation methods without added salt.
How does the DASH diet help manage heart failure symptoms?
The DASH diet emphasizes fruits, vegetables, whole grains, lean meats, and low-fat dairy products while limiting sodium intake. It can improve blood pressure and cholesterol levels, benefiting those with or at risk for heart conditions.
Are there any risks associated with following a very restrictive low-salt diet?
Severe sodium restriction could lead to complications such as hyponatremia (low blood sodium), affecting fluid balance in the body and potentially causing dehydration and other health issues.
Can I still enjoy flavorful meals on a reduced sodium diet?
Absolutely! Experiment with herbs, spices, lemon juice, vinegar, or salt-free seasonings to add flavor without adding extra sodium. Try garlic, onion, ginger, or fresh herbs like basil, cilantro, and parsley.
What’s the best way to track my daily sodium intake?
Keep a food diary noting all sources of sodium throughout the day. Use nutrition labels for packaged foods and apps that help monitor dietary intake. Aim for around 2,300 mg per day unless recommended otherwise by your healthcare provider.
How does sugar consumption affect heart health compared to salt?
While both excessive salt and sugar can negatively impact cardiovascular health, reducing sodium is often more directly linked to lowering blood pressure and improving outcomes in those with heart failure. However, limiting added sugars also contributes to overall heart health.



